Quality360
Revolutionizing Healthcare Analytics and performance
Achieve Compliance, Close Care Gaps, and Elevate Patient Outcomes
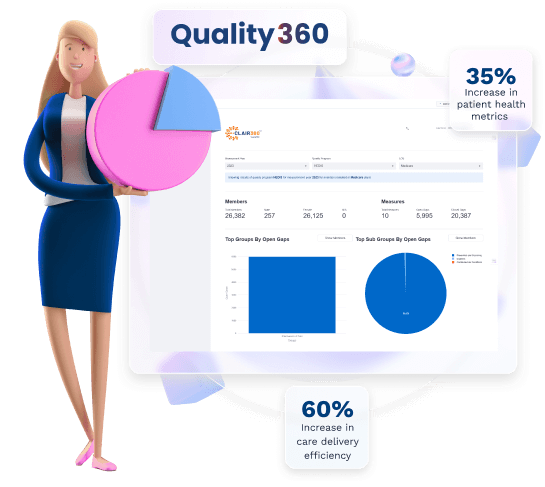
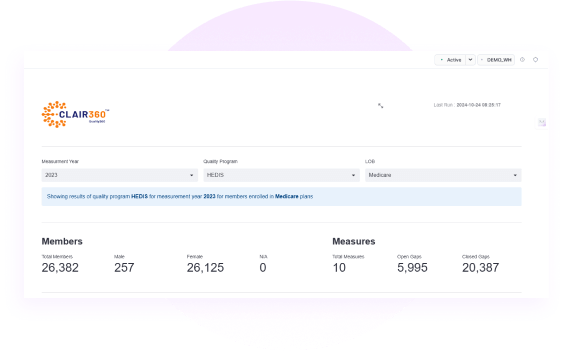
Quality360, a cutting-edge Snowflake Native App designed to transform the way payers and providers analyze patient data for HEDIS measures. Quality360, is an affordable tool to empower your quality program, which is also certified by NCQA for HEDIS measures. It offers a comprehensive suite of tools to streamline data analysis, facilitate data conversion, and ensure effortless submission to NCQA for star ratings.
Improvement in HEDIS scores with accurate data analysis and reporting
Reduce compliance issues with automated and NCQA-certified processes
Commitment to be HIPAA complaint with robust security measures
Decrease in operational cost through automation and streamlined workflow
Increase in reporting and data processing
Inefficient HEDIS Reporting and Compliance
Quality360 automates and streamlines HEDIS reporting, ensuring NCQA-certified compliance.
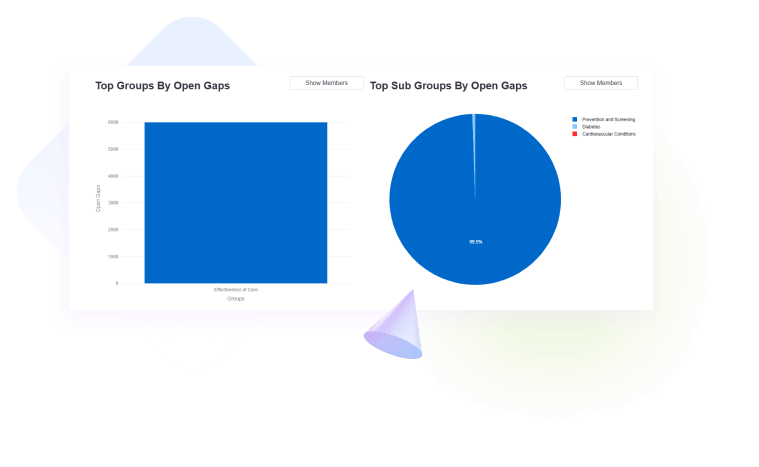
Inability to Close Care Gaps
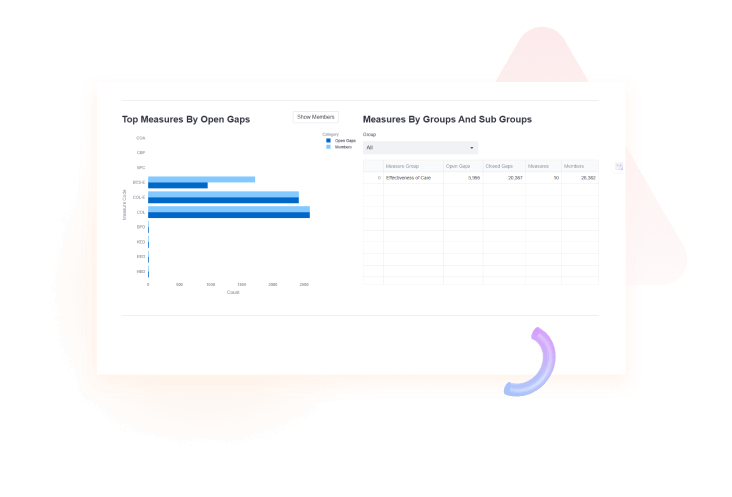
The tool provides real-time insights to identify and address care gaps swiftly. This enhances patient care quality and outcomes.
High OPEX and resource constraints
Quality360 minimizes manual effort and optimizes resources via automation. This leads to cost savings and improved efficiency.
Why Quality360
NCQA Certification
Quality360 is certified by NCQA, ensuring compliance with HEDIS standards for accurate and reliable reporting.
Real-Time Insights
The tool processes data instantly, providing up-to-date insights for identifying care gaps and improving patient outcomes.
User-Friendly Interface
Quality360 offers an intuitive admin setup, making it easy to configure and use without technical complexities.
Robust Security
With HIPAA-compliant security measures, Quality360 ensures the safety and confidentiality of sensitive healthcare data
Our Approach


Healthcare Payers (Insurers)
- To evaluate care quality, select top providers, and ensure regulatory compliance to enhance member satisfaction and health outcomes.
Healthcare Providers
- To monitor, and enhance care quality, meet contractual obligations, and attract patients by showcasing high-quality care.
Accountable Care Organizations (ACOs)
- To coordinate care, demonstrate value-based care excellence, and achieve financial incentives through quality and cost-effective care.
Managed Care Organizations (MCOs)
- To deliver high-quality, cost-effective care to members, meet regulatory requirements, and grow their membership base.
Third-Party Administrators (TPAs)
- To ensure compliance, provide data-driven insights, and optimize healthcare benefits for self-insured employers and insurers.
Quality Improvement Organizations (QIOs)
- To evaluate care quality, select top providers, and ensure regulatory compliance to enhance member satisfaction and health outcomes.
In healthcare, accurate data isn’t just important—it’s life-saving. Quality360 gave us the ability to clean up messy data and keep it consistent across systems and be complaint. Now, I can trust the numbers I’m seeing and make confident decisions for patient care.
CIO
Leading Healthcare Network
Managing HEDIS compliance was a challenge until we adopted Anblicks healthcare analytics solution. Its real-time data analysis and seamless reporting made it easier to identify gaps and improve care quality, all while ensuring compliance with NCQA standards.
Quality Assurance Manager
Leading Health Insurer

Trusted by






Empower Your Healthcare Program with Quality360
Understand how Quality360 can achieve compliance and close care gaps.